Definition
An inflammatory disease caused by the yeast Candida albicans and manifested clinically as erythematous papules and pustules that may become confluent to form plaques in the case of the former and erosions in the case of the latter. The nail unit may be affected by paronychia and the oral cavity by “thrush.”
Adjunctive Diagnostic Tests
Examination of skin scrapings by conventional microscopy in order to demonstrate budding yeasts with hyphae or pseudohyphae. Culture of tissue on Sabouraud’s agar enables colonies of yeast to grow.
Course
Lesions of candidiasis may be self-limited if the factor(s) responsible for their development is eliminated. For example, housekeepers and bartenders who have candidal intertrigo should keep their hands out of water as much as possible. Lesions of candidiasis sometimes persist and even worsen, such as in a person immunosuppressed consequent to long-term, high-dose therapy with corticosteroids administered systemically or secondary to a systemic disease like leukemia or lymphoma.
Integration: Unifying Concept
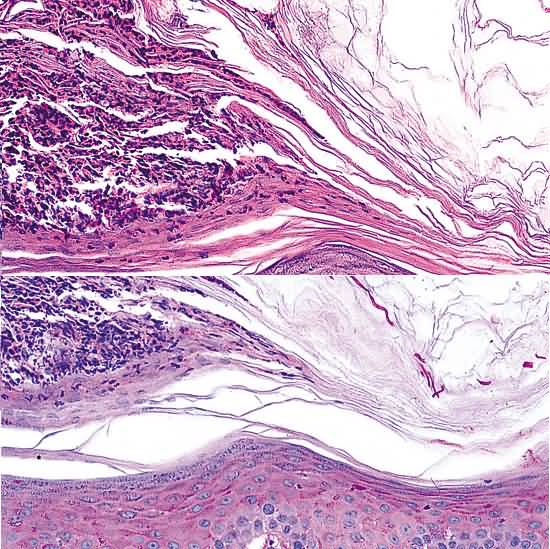
All the cutaneous, ungual, and mucous membrane lesions of the disease are a direct result of the effects of the yeast C. albicans. That organism flourishes in corneocytes of the stratum corneum and, occasionally, in those of the nail plate, but not in those of the hair shaft or inner sheath. It also luxuriates in corneocytes whose nuclei are retained in mucous membranes, such as those of the oral cavity and vagina. In patients who are severely immunosuppressed, candida may be carried by blood vessels to tissues throughout the body; in the skin, the yeast may proliferate wildly in the dermis and sometimes withOverview
C. albicans causes cutaneous disease in occluded, moist areas: the groin, axilla, inframammary areas, and the glans penis (in uncircumcised males). Diabetes, obesity, fecal and urinary incontinence, and immunosuppression are predisposing factors. The therapeutic strategy is to eliminate the pathogenic organism and to correct the factors that predispose the patients to candidal infection.
First Steps
1. If the skin is weeping, instruct the patient to soak in dilute Burow’s solution 1: 20 (1 tablet in a pint of water) twice daily for 15 minutes.
2. Prescribe nystatin ointment applied three times daily or an imidazole cream (eg, Clotrimazole, Nizoral or Spectazole, but not oxiconazole) applied twice daily to the affected area. If erosive lesions are present, the cream may cause burning.
3. Instruct the patient to dry the moist areas by exposing them to the air, and if appropriate, to keep stool and urine away from the skin.
4. Look for associated yeast vaginitis in cases of vulvar candidiasis in women.
5. If other risk factors are present (obesity, family history, symptoms, risk factors) evaluate the patient for diabetes mellitus and immunosuppression, especially HIV infection.
Subsequent Steps
1. Nystatin ointment or zinc oxide paste applied over the topical imidazole may enhance therapy by providing a protective barrier from sweat, urine, and stool.
2. Adding hydrocortisone 1% ointment to the anticandidal agent will speed healing and reduce symptoms more rapidly.
3. Men with balanitis may have partners with candidal vaginitis; the sexual partner also needs treatment.
4. Although cosmetically unattractive, gentian violet solution twice daily for 3 days is drying and has good anticandidal activity.
5. For severe unresponsive cases, oral fluconazole 150 to 200 mg/day for 1week is of benefit.
6. Preventive therapy includes keeping the area dry by wearing loose-fitting underwear and using topical drying bland powders (e.g., talc) or an imidazole-containing powder (e.g., miconazole nitrate).
Pitfalls
1. Do a KOH preparation prior to therapy to establish the diagnosis.
2. Secondary bacterial infection may require systemic antibiotics.
3. Avoid applying solutions to inflamed skin, as they will cause burning.
4. Refractory lesions may need a biopsy to rule out extramammary Paget’s disease, squamous cell carcinoma in situ (Bowen’s disease), and metabolic and other inflammatory causes of an intertriginous eruption.
in the epidermis and epithelial structures of adnexa.