Definition
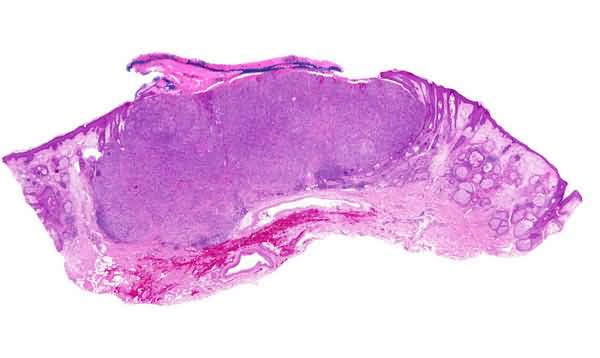
A malignant neoplasm made up of abnormal germinative cells analogous to those that compose the folliculosebaceous-apocrine germ in an embryo and that usually manifests clinically as a papule or nodule which may become ulcerated. On the basis of clinico-pathologic correlation, five distinctive types of basal-cell carcinoma have been identified, namely, nodular, superficial, morpheiform, fibroepithelial, and infundibulocystic.
Course
Five types of basal-cell carcinoma are recognizable on the basis of clinicopathologic correlation, namely, nodular, superficial, morpheiform, fibroepithelial, and infundibulocystic. As a rule, each of them grows slowly and does not do serious harm to a patient, but, episodically, a basal-cell carcinoma may kill by virtue of local destruction of tissue or, very rarely, of metastasis widely. It is the nodular type of basal-cell carcinoma, known also as noduloulcerative, that most often is responsible for extensive destruction of tissue locally and may even be associated with neurotropism. Most examples of so-called nodular basal-cell carcinoma remain papules, often ulcerated ones, for the lifetime of the person who bears them. In time, a papule may become a nodule and even a tumor. At times, a nodular basal-cell carcinoma can achieve gigantic proportions.
A superficial basal-cell carcinoma is usually flattish and, although it extends very slowly centrifugally, it usually remains flat or slightly elevated for a lifetime. Morpheiform basal-cell carcinoma, so named because it sometimes resembles morphea clinically, also grows slowly and rarely does serious damage. Because its borders are ill defined, however, this particular variant of basal-cell carcinoma tends to thwart excision completely and therefore is given to persist at the local site after incomplete excision of it. Fibroepithelial basal-cell carcinoma is a skin-colored indolent papule on a trunk that, for practical purposes, is innocuous. The same is true for the tiny papule on a face of infundibulocystic basal-cell carcinoma. That lesion rarely becomes larger than a tiny papule, growing extraordinarily slowly as it does for many years. It should be mentioned, parenthetically, that a nodular basal-cell carcinoma may develop in association with any of the other four types of basal-cell carcinoma, a fact that gives legitimacy to a unified concept of basal-cell carcinoma.
Overview
Basal cell carcinomas (BCCs) are best managed by persons expert in their recognition, natural history, and treatment. Failure to correctly manage tumors initially may lead to significant cosmetic deformity. General guidelines are given below, but the correct choice of therapy for individual lesions depends on age, sex, location, pigment type, and history of prior treatment. A biopsy to confirm the diagnosis should, in general, be performed before treating any lesion. The therapeutic strategy is always to remove or eradicate the tumor using a modality that offers the best chance of initial cure so that the likelihood of recurrence is minimized. While cosmetic considerations are very important, they should not govern the choice of the most appropriate and beneficial first therapeutic step.
First Steps
1. Surgical excision with a 2- to 5-mm margin of normal tissue is usually optimal. Send the specimen for pathologic evaluation for adequacy of excision.
2. In elderly persons (over 60 years) and in the debilitated, radiation therapy provides excellent results.
3. For superficial or small (under 2 cm) lesions of the trunk, curettage and desiccation (C & D) provides an acceptable cure rate and good cosmesis. C & D scars may be unsightly, and so this is not the preferred treatment for facial lesions.
4. Facial lesions over 1 cm in diameter that have been present for more than 2 years and lesions located in the temple, eyelid, medial canthus, nose, and nasolabial fold are more likely to recur. Consider them as potential candidates for micrographic surgery (Moh chemosurgery). In these cases surgical excision with micrographic control is preferred and radiation therapy is an alternative. C & D, in general, is not recommended.
5. All recurrent BCCs, BCCs whose margins are indistinct, morpheaform BCCs, and tumors that will require extensive reconstruction to repair the surgical defect are appropriately managed by micrographic surgery.
6. Superficial BCCs may be treated with imiquimod topically. The treatment schedule is once daily five times per week for 6 to 10 weeks.
Alternative Steps
1. For the rare patient who is unable to tolerate radiation therapy or surgery, local cryotherapy with thermocouple control may be an excellent alternative.
Subsequent Steps
1. Routine sun protection is advised for all patients.
2. Perform a complete examination of all sun-exposed skin on the initial visit and once yearly thereafter.
3. Patients using imiquimod should be seen after 4 to 6 weeks of treatment to determine if there has been an adequate response to eradicate the tumor. Treatment frequency may need to be increased to daily.
Pitfalls
1. Failure to correctly diagnose and treat BCCs may lead to additional scarring or cosmetic deformity. A biopsy of any suspicious lesion is required.
2. Choice of therapy on the basis of cosmetic considerations alone may result in failure to optimally treat the tumor with resultant recurrence. The eventual cosmetic result may be worse than if adequate treatment had been performed initially.
3. In some patients imiquimod by the standard schedule produces excessive local irritation, erosion, and potentially even ulceration and scarring. This excessive reaction is not required for adequate tumor eradication. If such a severe reaction occurs, the patient may stop treatment for 1 to 2 weeks and then resume treatment. This may need to be at a reduced frequency of three times per week. The total treatment course does not include these “holidays,” so the total treatment course may need to be extended.
4. Recurrence is possible after all forms of therapy, so any suspicious erythematous or papular lesions within or adjacent to the scar from treated BCCs should be biopsied.