Definition
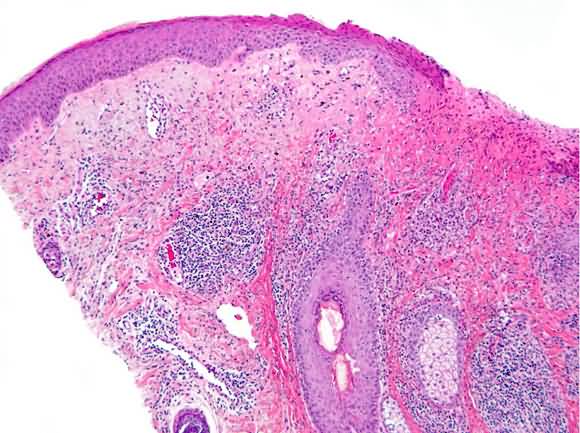
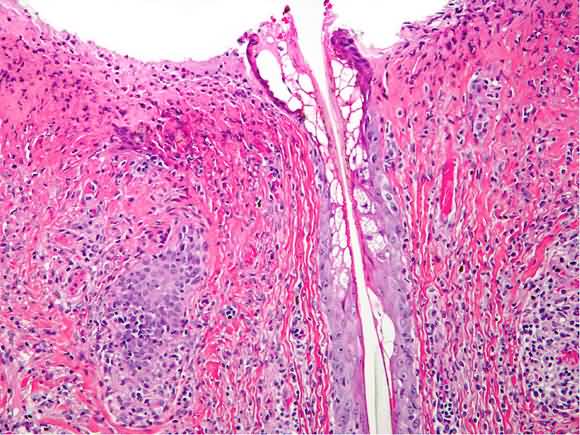
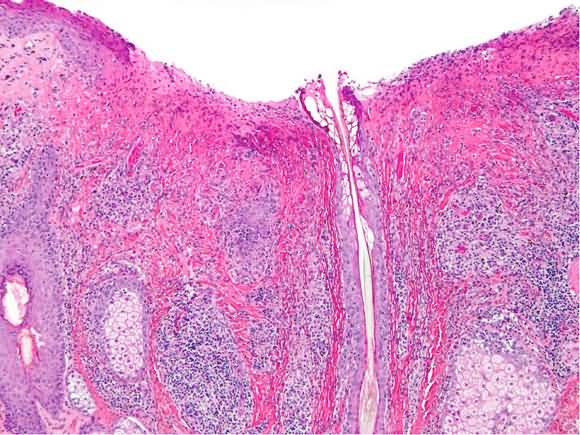
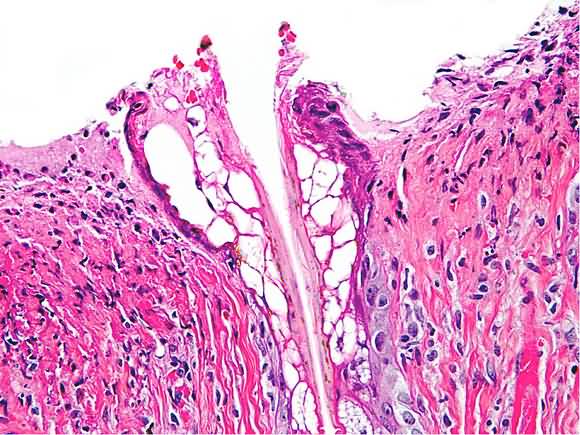
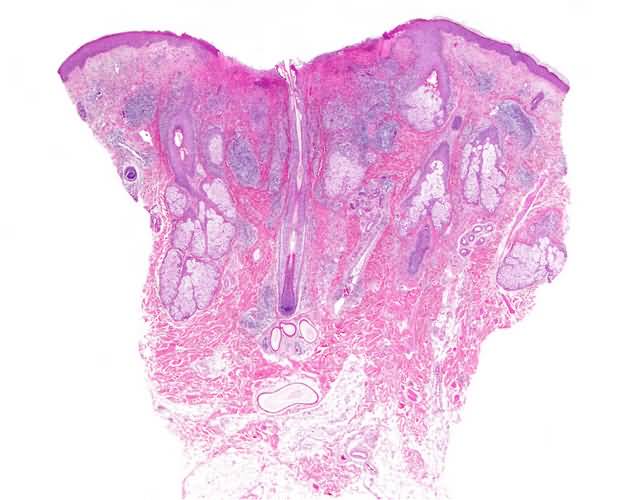
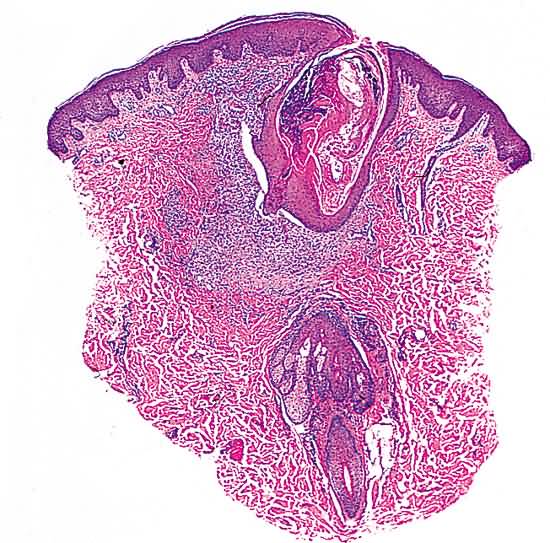
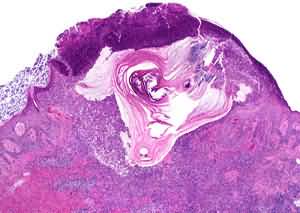
A disease of infundibulosebaceous units, especially infundibula, that may manifest itself solely as noninflammatory lesions, i.e., comedones and intact cysts, or as inflammatory lesions, i.e., papules, nodules, and pustules. The process may resolve without residua or with scars of different types, e.g., keloidal or atrophic, including cribriform. The condition usually affects adolescents, but may at times be seen in neonates and young adults.
Virtually every adolescent is affected by acne vulgaris, if only in a mild form. In adolescents and young adults it may persist for years, whereas in neonates it usually lasts for weeks or a few months. The most severe expressions of acne occur in males.
Course
Beginning with the flow of androgens at puberty, typical lesions of mild to moderately severe acne vulgaris in adolescents come and go for several years, usually disappearing completely and without residua, except at times for patulous infundibula on the nose and malar region. Episodically, the process is more fulminant and prolonged, conglobate lesions being long lasting and healing with unsightly atrophic scars. New lesions of acne keloidalis on a nape may continue to appear as the inflammatory process smoulders well into adulthood. Severe acne that occurs especially on the back in males often resolves with a type of anetoderma that presents itself as atrophic papules, and that is incorrectly designated “macular atrophy.”
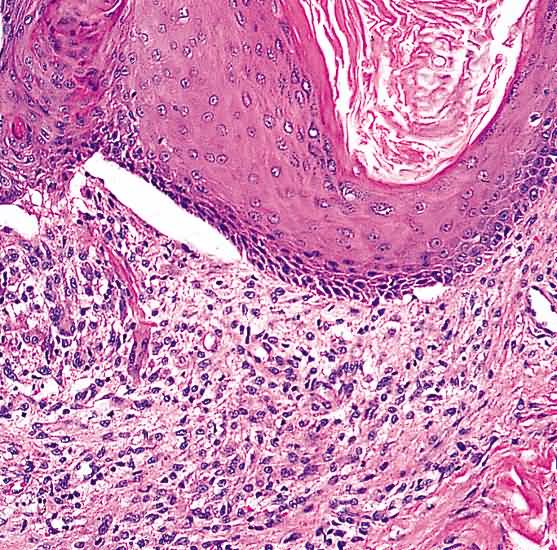
A comedo may become progressively larger and eventually be gigantic. In time, the ever-expanding plug of cornified cells causes the wall of an infundibulum to become so thin that eventually it is breached, spewing into the dermis cornified cells, sebaceous secretion, and microorganisms. This event sets in motion an inflammatory reaction marked initially by suppuration, then by granulomatous inflammation, and, in time, by fibrosis. A pustule situated within an infundibulum, in a fashion comparable to a comedo, may become so large that its contents are disgorged into the dermis where they inevitably induce granulomatous inflammation and, sometimes, fibrosis.
If the focus of suppuration in the reticular dermis (and, at times, the subcutaneous fat) becomes very large, a huge abscess forms and the destructive effects of products of the neutrophils that compose it lead invariably to extensive fibrosis. When the epithelium of infundibula and eccrine ducts then proliferates in pseudocarcinomatous fashion in an attempt to “wall off” the abscess, sinus tracts may come into being. If several contiguous abscesses have formed, each being positioned at the site of an infundibulum, the result may be sinus tracts that are interconnected. That phenomenon resolves with extensive fibroplasia.
Acne vulgaris may consist only of comedones, but in most patients, comedones are joined by reddish papules and pustules. That very common expression of acne vulgaris does not, as a rule, resolve with scars. If, however, abscesses form and especially if the process eventuates in draining sinuses, severe scarring is a certainty. Whereas pustules of acne vulgaris may begin to wane in days, abscesses that are followed by granulomatous inflammation and fibrosis may not resolve completely for many months.
Grade I to II Acne First Steps
1. Primarily comedonal acne is best managed with tretinoin or another primarily anticomedonal agent (e.g. adapalene).
2. Benzoyl peroxide gels or lotions (2.5% to 10%) used once daily have mild anticomedonal effect and are good initial treatment for mild acne. It is especially useful if there is a mild pustular component.
Alternative Steps
1. The combination of benzoyl peroxide in the morning and tretinoin or adapalene at night may be used when either agent alone fails. Irritation potential is also additive.
2. Mild comedolytic effect can be achieved by use of products containing salicylic acid 2%.
3. Removal of comedones with a comedone extractor by the patient or careprovider accelerates clearing. Topical anticomedonal agents, especially tretinoin, loosen comedones, enhancing their removal.
Subsequent Steps Positive initial response
Once the initial response is noted, continue treatment for 3 months. After this period, the frequency and strength of medications may be decreased at monthly intervals to a maintenance dose. Stopping therapy will usually result in a flare in 3 to 6 weeks if the tendency for acne is still present.
No initial response
1. Consider a topical benzoyl peroxide/topical antibiotic combination in the mornings and tretinoin or adapalene nightly.
2. Add an oral or topical antibiotic.
3. Isotretinoin may be considered in severe acne scarring cases that have not responded to the above therapies.
Pitfalls
1. Treatment of acne prevents new lesions, and, therefore, must be applied to the whole potentially affected area, not just to the lesions.
2. Do not consider any therapy ineffective sooner than 1 month. Be patient. Continue any effective treatment for 3 to 6 months before slowly tapering off until the level of therapy is at the minimum required for maintenance.
3. Acne will often flare after 2 to 3 weeks of tretinoin use. Warn the patient about it. It will resolve within 6 to 8 weeks. Tretinoin flares can be prevented by starting the applications every 2 to 3 nights, only for the first month, and using a topical antibiotic in the mornings.
4. Tretinoin may induce photosensitivity, so prescribe its use only at night, and encourage the use of a noncomedogenic sunscreen.
5. Overzealous use of tretinoin and/or benzoyl peroxide products will lead to skin irritation. Only small amounts of tretinoin (pea-sized for the entire face) should be applied. Visible irritation is not required for tretinoin to be beneficial.
6. Facial comedones (especially of the forehead) are often related to oily hair care products. Their use must be curtailed for the acne to improve.
Grade III to IV acne
Initial treatment is divided into that for mild to moderate cases (usually nonscarring and facial) and that for moderate to severe cases (potentially scarring and often truncal). The first steps are to cool down the acne, reducing the inflammatory lesions. After a few weeks, topical tretinoin or adapalene is added. The use of anticomedonal agents initially may flare the acne too significantly to be tolerated by the patient. Eventually, however, all patients should be on tretinoin or adapalene chronically for maintenance.
First Steps Mild to moderate cases
1. A topical antibiotic (erythromycin 2% or clindamycin 1%) in lotion or gel form, in combination with benzoyl peroxide applied twice daily. These may be applied as two separate products or as a combination product. If separate products are used, the benzoyl peroxide is applied only once daily.
2. Low-dose oral antibiotic (tetracycline 500 mg twice daily or doxycycline 100 mg every day. Moderate to severe cases
1. An oral antibiotic (tetracycline 500 mg or doxycycline 100 mg twice daily), and
2. Benzoyl peroxide gel or lotion (2.5% to 10%) applied to the affected area. Patients with trunk lesions may find a wash in bar or lotion form to be an easier way to use benzoyl peroxide.
3. Use of vitamin A acid cream (0.025% for the face, 0.1% for the trunk) or gel (0.01% for the face, 0.025% for the trunk) initially every other night may be added to the above therapeutic regimen. Encourage nightly application as tolerated. For trunk lesions, the tretinoin solution is an easier form of application.
Alternative Steps Antibiotics
1. Minocycline 50 to 200 mg/day is more effective than tetracycline or erythromycin. Cost limits its firstline use.
2. Trimethoprim-sulfamethoxazole 1 double-strength tablet once or twice daily may control acne when other antibiotics fail. Its high rate of allergic reactions (6%) limits its use.
3. Cephalexin 500 mg three times a day or cefadroxil 500 mg two times a day are alternatives for patients allergic to the above antibiotics.
4. Clindamycin 150 to 600 mg/day may also work when other antibiotics fail. Diarrhea (potentially life-threatening) limits its use.
Anti-inflammatory drugs
1. Nonsteroidal anti-inflammatory drugs (ibuprofen, naproxen) improve the inflammatory component. They are useful adjuncts to antibiotics.
2. Corticosteroids a. Short courses (7 to 10 days) of systemic steroids (prednisone 20 to 40 mg/day) will abort flares at critical times (weddings, proms, interviews, etc.).
b. Intralesional injection of small amounts of triamcinolone acetonide (2.5 to 5.0 mg/cc) will lead to rapid resolution of cysts. Local steroid atrophy may result, so counsel the patient appropriately. The atrophy usually resolves in 3 to 6 months.
Subsequent Steps Positive initial response
1. Continue the treatment regimen for 3 months.
2. Tretinoin or adapalene cream or gel applied nightly is useful even in the most severe cases. Due to its potential to irritate and tendency to flare the acne, it is often begun 4 to 6 weeks after other treatments.
3. Topical antibiotics, although not initially effective, may be gradually substituted for low-dose oral antibiotics in some cases.
4. Premenstrual flares and flares during examinations and other stressful situations are common. Treat with additional oral antibiotics for 1 to 2 weeks before and 1 to 2 weeks after the potentially flaring episode. Systemic steroids as described above may be useful in flares which are unlikely to recur (after a wedding, for example).
No initial response
1. Increase the dose of antibiotic: tetracycline 500 mg or doxycycline 100 mg twice a day, or
2. Switch to an alternative antibiotic (minocycline or trimethoprim sulfamethoxazole).
3. Add tretinoin or adapalene gel or cream nightly.
4. In women, consider Spironolactone 50 mg to 100 mg daily, with or without oral contraceptive pills.
5. Isotretinoin treatment. While approved only for unresponsive nodulocystic acne, isotretinoin will improve all forms of acne. The severe psychological impact of acne on the patient’s quality of life should not be underestimated. A long-term remission can be obtained in between a third and two-thirds of patients treated. Patients at risk for pregnancy or depression have a higher threshold for treatment due to potentially more severe complications. Treatment should be started at lower doses in patients with severe nodulocystic acne to avoid acne fulminans. The usual starting dose is 20 to 40 mg. The treatment course should be at least 5 months and should reach the desired full cumulative does of 120 mg/kg. Most patients tolerate between 0.75 mg and 1.0 mg/kg/d with minimal side effects. Oral antibiotics can be continued during the first month or two of isotretinoin therapy to avoid flares.
Pitfalls
1. Many failures in acne treatment are related to inadequate patient education. The patient must be instructed on what causes acne, how the recommended treatments work, and exactly how the prescribed medications are to be used.
2. External factors that trigger the acne must be removed for therapy to be effective. The three major ones are acnegenic medications (e.g. topical and systemic steroids), comedogenic cosmetics and creams, and friction.
3. Even the most effective medications take 4 to 8 weeks to work and sometimes even longer. Be patient.
4. If acne fails to respond, perhaps it is not acne. Consider chronic folliculitides of other causes, and other diagnoses.
5. Female patients with acne, especially if they also have evidence of hirsutism, may have a hyperandrogenic state. Endocrine evaluation and correction or suppression of the condition may lead to improvement of the acne when other approaches fail.
6. Ask female patients whether they are pregnant or plan to get pregnant. Certain acne medications (e.g., tetracycline and isotretinoin) are contraindicated in pregnancy.
7. Ask female patients whether they are taking OCPs. Certain OCPs can exacerbate or cause acne. In addition, tetracycline and other antibiotics have been reported anecdotally to decrease the efficacy of OCPs, so patients must be counseled appropriately.
8. Patients taking chronic antibiotics, especially if using topical antibacterial soaps as well, may develop a gram-negative infection of the face that looks like acne. Lesions must be cultured, and appropriate antibiotic therapy or isotretinoin should be prescribed.
9. Many patients treated with isotretinoin receive inadequate courses and have a reduced likelihood of a long-term response. Once the decision to use isotretinoin has been made, the patient and prescriber should agree to a full course of therapy, by total dose, not time of treatment.
10. Patients with mild dyslipidemias may develop marked hypertriglyceridemia and its complications (pancreatitis). Elevation of hepatic enzymes and, much more rarely, hepatitis may also occur with isotretinoin treatment. Less commonly, frank diabetes mellitus should develop.
11. Depression is a possible dose-dependent side effect of isotretinoin treatment. The patient’s mental status must be checked at every visit. Patients with pre-existing depression must be carefully evaluated before starting isotretinoin, and consideration should be given to following them in consultation with a mental health professional.
12. All patients treated with isotretinoin should go through an FDA-approved screening program before starting treatment, and should be monitored in accordance with FDA guidelines.
13. Effective contraception must be insured in all potentially fertile female patients treated with isotretinoin. Monthly pregnancy tests during treatment are required.